Neurosurgery Mission to Dar es Salaam and Bugando, 2011 (Part 2)
Part 2: Return to Bugando Following our stay in Dar Es Salaam, a team comprised of three neurosurgical attendings, two neurosurgical residents, two attending anesthesiologists, a nurse anesthetist and OR nurse from the Barrow Neurological Institute in Phoenix, Arizona and Weill Cornell Hospital, New York, traveled to Mwanza on Lake Victoria to continue the mission to build a self-sufficient neurosurgical practice at Bugando Hospital. The team was met by familiar faces including the chair of surgery Dr. Mahalu, Dr. Isidor Ngayomela and Dr. Emmanuel Kahamba, as well as many new residents interested in neurosurgery. Once again we found the surgical instruments and drill previously donated to be in good working order and we were able to utilize them in numerous cases over the course of the week. A typical day at Bugando hospital started at 7:30am in the halls of the surgery ward. Residents that were on-call overnight presented their admissions to the surgical team. Frequently, these patients suffered brain injury from a trauma. An open discussion about the physical exam findings, localization of injury and appropriate management would follow. After presentations we walked the wards to examine patients and finalize our treatment plans with the team before heading to clinic or the operating theatres. During our visit we saw many different pathologies but it was evident that trauma, hydrocephalus and myelomeningoceles were some of the most prevalent neurosurgical issues. It was great to see that many of the surgeons there were adept at shunt placement and getting proficient at basic trauma surgery and repair of myelomeningoceles; evidence that work done on previous missions has already had an impact! We focused on these cases working side by side with Drs. Emmanuel and Ngayomela in more complicated cases and introduced basic procedures like shunt placements and burr holes for evacuation of traumatic hematomas to those new to neurosurgery. Case 1The first case was a 40 year old gentlemen with months of progressive right sided weakness and headaches. He had a CT scan with contrast prior to our arrival. The patient had a very large mass near the dominant motor cortex that was causing significant compression of the brain. He was taken to the OR where Drs. Härtl, Lockhead and Kahamba performed a craniotomy for biopsy and possible resection. Upon opening the dura a firm, yellow mass was encountered that was easily separated from the brain tissue consistent with a TB granuloma. They were able to remove the entire abscess and the patient recovered well. His strength improved tremendously after surgery and he was discharged from the hospital after three days. The final pathology results indeed confirmed the diagnosis of a TB granuloma.  CT scan demonstrating brain lesion
CT scan demonstrating brain lesion
 Tuberculoma resected from the brain of the patient in Bugando
Tuberculoma resected from the brain of the patient in Bugando
Case 2The second case was a 21 year-old male admitted the previous night after being assaulted with severe injuries to his head. Plain x-rays revealed depressed skull fractures and visible lacerations to the left scalp. Patient was obtunded and hemiplegic on the right side. A decision was made to take the patient to the OR for washout and exploration of the wound. Multiple depressed skull fractures and bony fragments were removed from the brain and the lacerations were cleaned and closed. A drain was placed to measure intracranial pressure and the patient was moved to the ICU. His intracranial pressure was managed medically and the drain was removed on day 5. The patient was becoming more alert and was taken off the ventilator by the end of our visit. As per latest report he made an excellent recovery.
 Young surgeons, students and medical staff at Bugando watching Dr. Robert Galler from New York, Dr. David Rubin and local neurosurgeon trainee Dr. Kahamba perform a debridement and decompressive craniectomy in a patient with depressed skull fracture from a machete injury
Young surgeons, students and medical staff at Bugando watching Dr. Robert Galler from New York, Dr. David Rubin and local neurosurgeon trainee Dr. Kahamba perform a debridement and decompressive craniectomy in a patient with depressed skull fracture from a machete injury
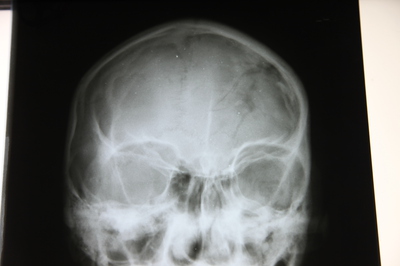 Skull x-ray demonstrating depressed skull fractures
Skull x-ray demonstrating depressed skull fractures
Case 3The surgical ward was overflowing with kids suffering from hydrocephalus. Hydrocephalus is the inability to resorb the normal fluid produced by the brain, which untreated, can lead to significant increase in head size, discomfort, neurological deficit and even death. We stressed the importance of frontal shunt placement for these patients, which decreases the risk of wound breakdown, infection, and shunt failure, and helped the Bugando surgeons get comfortable with this technique. It is our hope that this simple change will decrease the rate of shunt malfunctions and need for future revisions. 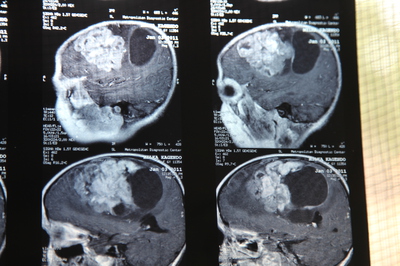 Brain MRI scan of a young girl demonstrating large brain tumor
Brain MRI scan of a young girl demonstrating large brain tumor
 Neurosurgery trainee Dr. Emmanuel Kahamba operating on a spinal fracture. Spinal fractures occur frequently and previously went untreated
Neurosurgery trainee Dr. Emmanuel Kahamba operating on a spinal fracture. Spinal fractures occur frequently and previously went untreated
 Orthopedic surgeon and spinal surgery trainee Dr. Isidor Ngayomela operating on a complex spinal case with Cornell neurosurgery resident Dr. Lewis Leng and Cornell operating room nurse Lindsay Posner during our Bugando mission in 2010
Orthopedic surgeon and spinal surgery trainee Dr. Isidor Ngayomela operating on a complex spinal case with Cornell neurosurgery resident Dr. Lewis Leng and Cornell operating room nurse Lindsay Posner during our Bugando mission in 2010
In clinic, we were surrounded by patients and medical students that were eager to learn. Patients were seen with the medical students and physical exams, approach to patient history and pathology were discussed in detail. It was a great opportunity for the medical students at Bugando to ask questions and practice performing neurological exams.
Overall, it was a very busy but rewarding week. Every effort was made by our team to integrate ourselves into the Bugando culture and workplace, not operate as an independent team. At the end of our trip we received a lot of positive feedback from the residents, attendings and staff at Bugando Hospital. They were very pleased with the teaching approach that Dr. Härtl and others had implemented there. When we did get time away from the hospital we were able to take some amazing day trips to the plains of Serengeti and the beautiful beaches of Zanzibar.
Weill Cornell Medicine Center for Global Health
Center for Global Health
420 East 70th Street, 4th Floor, Suite LH-455
New York, NY 10021
Phone: (646) 962-8140
Fax: (646) 962-0285

